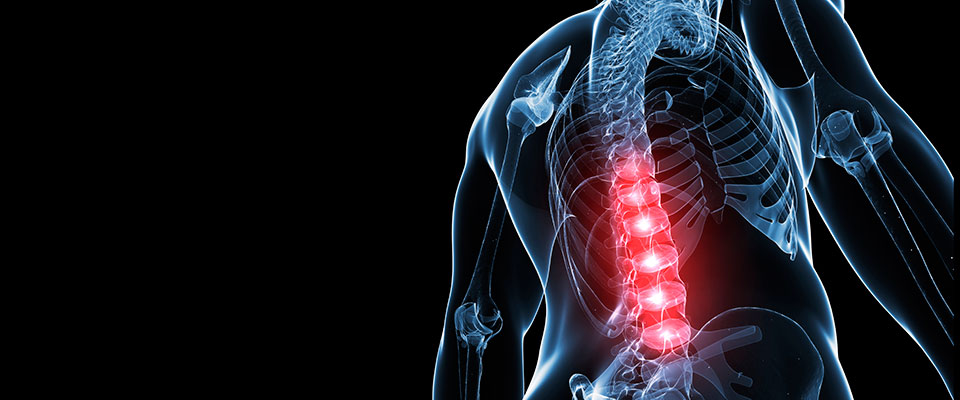
Anterior Lumbar Interbody Fusion (ALIF)
This operation involves placement of bone graft between the vertebrae, which are then secured by instrumentation (plates, screws, cages) with the goal of ultimately developing a solid bony connection (‘fusion’) between the vertebrae to prevent painful movement from occurring.
In this procedure the spine is approached from the front (‘anterior’), through a 10-12cm incision in the lower abdomen. The surgery is performed in conjunction with a vascular surgeon who helps navigate around the big blood vessels that lie in front of the lumbar spine.
Before Surgery:
The operation will be performed at St Georges Hospital. We will send out a preadmission pack for you to complete prior to your scheduled date.
Do I need to stop any medications prior to surgery?
If you are taking medications that affect your bleeding tendency like Aspirin, Warfarin, Clopidogrel or Dabigatran these may need to be discontinued at least 5 day prior to surgery. Please advise my personal assistant (Amanda) if this pertains to you. Other medications should be taken as normal unless advised otherwise.
The Day of Surgery:
How long prior to surgery do I need to avoid food or drink?
You will need to stop eating and drinking (other than water) 6 hours prior to your surgery. You should stop drinking water and chewing gum 2 hours prior to your surgery.
What type of Anaesthetic is given?
In all patients a general anaesthetic is given meaning you will be completely asleep for the duration and will have no memory of the procedure.
How long will the operation take?
The surgery typically takes 2 hours. You will be looked after in the recovery area for a further 60 - 90 minutes after the surgery has finished until the effects of the anaesthetic wear off before you return to the ward.
How long will my scar be?
Typically the scar measures 10-12cm in length, is horizontal and placed in the lower abdomen. If you have had a previous caesarean section typically the same scar will be re-used. Frequently a second scar, 4cm in length is placed over the rim of the pelvis (‘iliac crest’) through which bone healing cells (bone graft) are harvested and placed into the space between the two bones (‘vertebrae’) to aid healing (‘fusion’).
How long will I stay in hospital?
On average a 3-night stay in hospital is anticipated but this is dependent on a number of factors including you comfort levels mobilising.
How will my pain be controlled after the surgery?
At the end of the operation the surgical sites are injected with local anaesthetic to help control pain levels in the first 8 hours.
Post surgical pain is controlled with a combination of medications. Some of these, particularly in the first 24 hours, are given intravenously in a manner that you control with a push of a button (called ‘Patient controlled Analgesia or ‘PCA’). Others medications to control pain are available by mouth.
Another option that may be utilized involves using a catheter (thin plastic tube) placed under the incision. The nurses inject local anaesthetic into this a regular intervals post op to help control the pain for the first 24 to 48 hours.
What are the risks of surgery?
While surgery has an excellent ability to improve your symptoms some risks exist.
These include:
- Wound infection (<2%)
Which may require antibiotics or, if severe, further surgery to irrigate the area.
- Bleeding
In rare circumstances bleeding from the major artery and veins that supply the legs and pelvis, that lay in front of the spine, can occur. The vascular surgeon is on hand to address this if it occurs. A blood transfusion may be required if the bleeding is significant enough (<3%). In very rare (<1%) circumstances the bleeding can be life threatening.
- Nerve damage
The nerves that supply leg movement are not under direct threat during the surgery. Damage to these nerves is rare (<1%)
- Retrograde ejaculation (5-10%)
In males the operation can lead to a condition known as retrograde ejaculation (1%). Very small nerves that lay directly over the disc control the direction of the ejaculate. If damaged, the sperm travels backwards into the bladder rather than outward.
This results in infertility - but does not result in impotence or change significantly the sensation of ejaculating. In some cases this issue resolves in 6 to 12 months.
- A solid fusion does not occur (called a ‘non-union’ or ‘pseudoarthrosis’)
In ~5% of cases despite setting the scene with bone graft and stabilisation the body doesn’t form a solid connection between the two vertebrae and over time movement continues. If this occurs symptoms may persist. This scenario is commonly address by adding additional fixation / screws put in via the posterior approach – i.e. from the back.
- Persistent symptoms (~10%)
While persistent symptoms can occur from a non-union (as described above) in other cases, even when the operation goes technically well, patients may have residual symptoms. The potential reasons for this are many and complex, for example it’s possible that other sources of back pain co-exist in your back that were under appreciated.